Meet GBT, the game-changing and evidence based protocol for better oral care created by leading experts, making thousands of clinicians love their job even more. Bye-bye stress, bye-bye biofilm.
GBT the one and only
GBT the one and only
A healthy mouth for life. By focusing on prevention with effective, painless oral prophylaxis, nothing stands in the way of strong, healthy teeth, gums, and long-lasting oral health.
Discover the GBT protocol
_1759151034.webp)
Best clinical protocol
= best clinical results
Happy patients
Based on a 500k person survey
Successful practices
Good money for good work
Referral to dentist
Patient satisfaction
Recall rate

GBT reduces the risk of caries and gum disease by removing all biofilm. With conventional professional teeth cleaning, only 50% of oral biofilm is removed in hard-to-reach areas.
Discover the GBT Protocol
Do good, feel good
Hans L. - Switzerland
I did a dental cleaning session with the GBT protocol and I found it amazing! Quick, painless and totally effective procedure. I want to do it every week for the result provided, far superior to a normal prophylaxis.
Charlotte M. - France
The treatment was for my 3 children, 11, 12 and 14 years old. They were all anxious but after GBT they want to come back as it was so smooth and pleasant without any pain. No fear from prophylaxis anymore!”
Sabine K. - Germany
I’m so happy with GBT, I could not accept any other teeth cleaning method anymore. Due to GBT I see my dentist regularly and gladly for my prophylaxis. And each time I leave the practice I’m happy with my clean and brilliant white smile! To me, prophylaxis with GBT has become a great experience and I clearly recommend it!

Revenue Calculator
GBT is backed by clinical and scientific evidence.
Putting more smiles
on people every day.

Making the world smile, day by day.
See More
GBT certified clinic in Atrecht, Netherlands.
See More
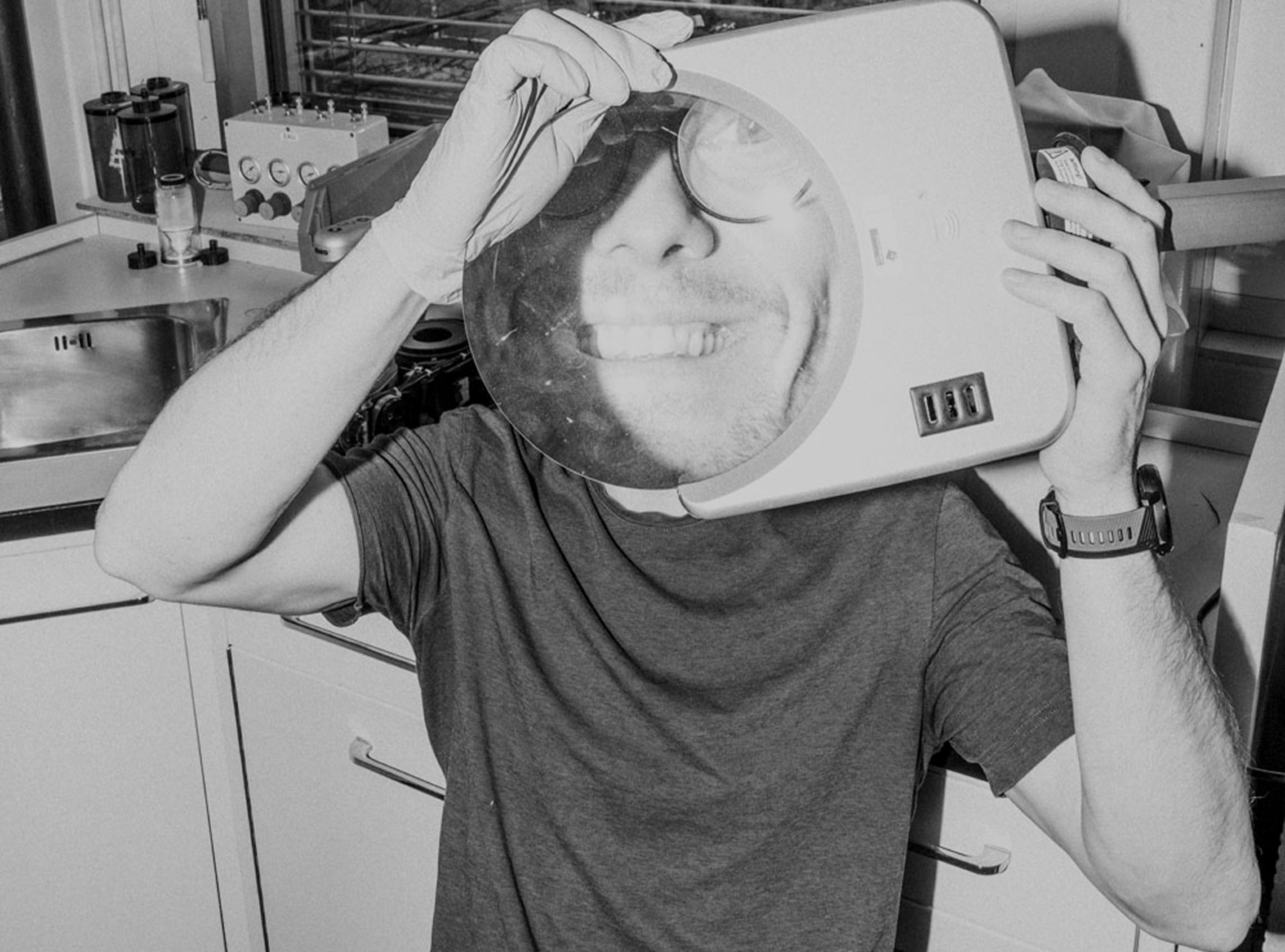
After a GBT treatment. I Feel Good.
See More

Your everyday reason to smile.
See More
Smile is in the air.
See More
EMS summer party!
See More

Daily doses of happiness.
See More

Smiles? Yeah, we’ve got those. Every day.
See More
GBT certified clinic in Lisbon, Portugal.
See More
GBT summit in Poland.
See More
I Feel Good at IDS.
See More
SDA training centre in Australia.
See More
SDA training at our HQ in Nyon, Switzerland.
See More
EMS summer party.
See More